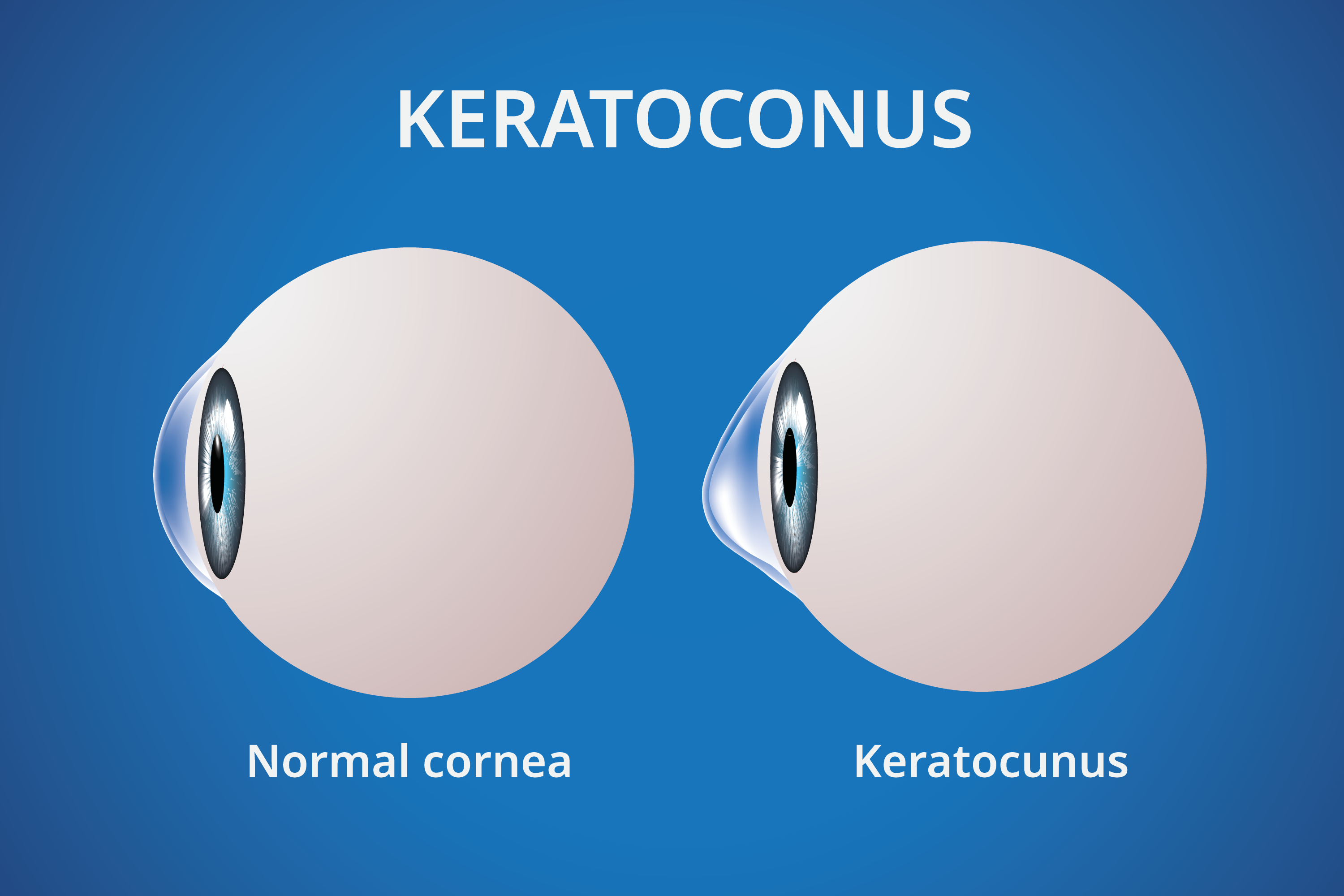
Keratoconus is a condition that affects the shape of the cornea, causing it to thin and bulge outward into a cone-like shape. It can lead to blurry vision, increased light sensitivity, and frequent prescription changes. While it most often begins in adolescence, new research is helping us understand how this condition behaves across different age groups and health backgrounds—and even how it might be managed more effectively.
Here are three important updates from recent keratoconus studies:
A recent pilot study from Italy revealed exciting news: adolescents with keratoconus and low vitamin D levels showed slower disease progression when they received vitamin D supplements.
Over the course of a year, these teens had more stable corneal shape and vision, and showed lower levels of inflammation and collagen breakdown in the body. This research suggests that vitamin D could play a protective role for the cornea—particularly during those teenage years when keratoconus often worsens.
What this means for you: If you or your child has keratoconus, it might be worth checking vitamin D levels. Good nutrition and appropriate supplements could be part of your care plan. The best way to check vitamin D levels is through a simple blood test called the 25-hydroxy vitamin D test (also written as 25(OH)D). Here’s how it works and what to know:
🧪 What it Measures
It measures the total level of vitamin D in your blood, including both D2 (from food) and D3 (made in your skin and from supplements).
📊 What’s a Normal Level?
Deficient: Below 20 ng/mL
Insufficient: 20–30 ng/mL
Sufficient: 30–50 ng/mL (ideal for most people)
Potentially too high: Over 100 ng/mL
👩⚕️ Where to Get It Done
Primary care physician: Can order the test during a routine check-up
Pediatrician: Can order it for teens or children
Direct-to-consumer labs: Like QuestDirect or Everlywell, for at-home testing
Specialist clinics: Especially in functional medicine or endocrinology
📌 Why It Matters for the Eyes
In patients with keratoconus, low vitamin D has been linked to faster progression of the condition. Ensuring vitamin D levels are adequate might offer some protective benefit—especially for adolescents.
Another study has found a strong genetic link between allergic asthma and the development of keratoconus. In fact, individuals with allergic asthma were more than twice as likely to develop this corneal condition.
Interestingly, other allergic conditions like eczema and conjunctivitis did not show the same direct connection.
What this means for you: If you or your child has allergic asthma, make sure to schedule regular eye exams. Catching early signs of keratoconus can make a big difference in long-term eye health.
Most people associate keratoconus with younger patients, but a new study in Iran discovered that over 5% of people aged 60+ showed signs of keratoconus, with rates climbing even higher among those over 80.
Risk factors included lower education levels and jobs involving a lot of time outdoors—possibly due to more UV exposure or frequent eye rubbing.
What this means for you: If you’re over 60 and planning for cataract surgery or noticing new vision changes, corneal imaging might be a smart step. Even subtle signs of keratoconus can affect surgical planning and outcomes.
These studies are helping us better understand keratoconus and how we might manage or prevent its progression—at every age. Whether you're a parent of a teen with allergies or an older adult noticing new vision changes, staying proactive with eye care is key.
Have questions or want to schedule a corneal evaluation? We’re here to help.
📞 Call or text us today to book your appointment!
🧡 Your vision is our priority—at every stage of life.